Ethics in Mass Spectrometry
Columnist Ken Busch discusses the lack of a formal ethics training program for physical scientists and the need for some type of self-regulation within the field.

Physical scientists, including mass spectrometrists, have fewer opportunities for ethics training specific to their field. Such training is not required in most scientific professions for graduate degrees or certification, nor for membership in most scientific societies. For example, although the American Chemical Society has long had a "Code of Conduct," it was only after extended debate that the society recently established a Committee on Ethics. In this overview, we draw the distinction between broad ethical issues, and those concerns allied with the topic known as responsible conduct of research. Responsible conduct of research covers expected practices in research and analysis meeting the standards of scholarship, including assurances of data integrity, the honest interpretation and reporting of results, and respect for the intellectual contributions of colleagues. Allegations of research misconduct can therefore involve issues of plagiarism, fabrication, and falsification, and debates about ownership of intellectual property. Training in the responsible conduct of research encompasses topics as diverse as good laboratory practice, means of provision of certification and assurances for data and results, and continuing technical training and maintenance of expertise. Ethics is a broader topic that includes the responsible conduct of research along with issues such as measurements pertaining to human subjects or human health, personal morals and beliefs, conflicts and their resolutions, and scientific philosophy in the widest possible context. An example of the last is the current debate about the ethics of stem cell research. At the same time, ethics plays out in very specific issues that can arise in the daily professional practice of individuals. Ethics plays out in decisions that should be made carefully and with a full understanding of issues involved. It is for this reason that this introduction to ethics in mass spectrometry (MS) appears here.

Kenneth L. Busch
At some point during our technical education as mass spectrometrists, we should have learned the rudiments of the responsible conduct of research. We should, for example, design our experiments to be clear and unambiguous; record data completely and impartially; consider alternative hypotheses; and retain data that somehow might not fit into those hypotheses that we formulate. We should keep proper and complete laboratory notebooks and records, and we should maintain proper instrument performance and calibration. Our research experiences, as both undergraduate and graduate students, provide us with examples from our mentors and colleagues as to how to accomplish these tasks in the chaotic world of research. It should be no surprise that in an industrial career, the emphasis on careful and complete record keeping becomes even more stringent. If you actually read the full employment contract, you will find that industry pays very careful attention to issues such as ownership of intellectual property. You might be interested to look at postemployment restrictions. Certainly, the requirements for responsible conduct of research are not new to mass spectrometrists, although the complexity of each individual issue has increased over the years, and the amount of regulation has increased. Public instances of misconduct by scientists usually result in more oversight and more regulation.
New and specific to MS research are broader ethics issues that extend past the responsible conduct of research. Many of these issues relate to medical research and findings that might have been predicted, but which are now more cogent. The decades-old dream of medical screening using mass spectrometry is now on the cusp of reality. The extraordinary advances that biological mass spectrometry has made over the last 20 years have revealed new ethical portals and dilemmas. One need only scan the titles of recent papers or publications dealing with the discovery of biomarkers to see hints of these ethical issues. The titles might suggest implicitly that diagnoses can be made based on MS data, or that disease markers are unambiguously revealed with the proper sample and the appropriate analysis. Table I lists some partial titles of recent presentations at 2008 conferences on spectroscopy, including MS. These titles convey a certain meaning to the professionals in attendance at the meeting, who implicitly add a "potential" or a "possible" modifier into a title. But the titles might convey other more certain and less nuanced meanings to the public, especially the members of the public searching for information on just these topics. A phrase such as "bench to bedside" brings to the public's mind the magical, but still fictional, abilities of Star Trek's medical tricorder. As professionals we know that these capabilities are still in the future. But the public does not.
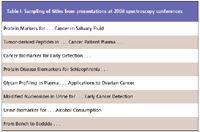
Table I: Sampling of titles from presentations at 2008 spectroscopy conferences
At the 2008 conference of the American Society for Mass Spectrometry, Steven Carr offered a practical overview, concluding that few early "markers" have to this point proved genuine or useful (1). However, some do, and more will, with added research. As a professional group, and a professional society, we will also have to learn to properly manage the announcement of putative markers, and confront the realization that false hopes can be generated by such announcements. As individual researchers, we must be prepared to assist in navigating the regulatory environment for such tools, and mute our usual impatience with it. Finally, as responsible scientists, we should be aware of the ethics issues involved in research that directly impacts individuals. Therefore, in this introduction to ethics in mass spectrometry, we touch briefly on the topics of institutional review boards and the control of MS data through informed data management.
As a mass spectrometrist in the United States, if you work with the analysis of samples derived from an individual person, then your research work will have fallen under institutional review board (IRB) jurisdiction, and must have undergone IRB review. This board is part of the process to provide protections for human subjects involved in research. You can be sure that your institution has an IRB or access to one, and that your institution offers IRB training. Make some time and take it. For those not usually directly involved with IRBs, misconceptions abound, and the consequences of misconceptions can be serious. Research projects can be terminated abruptly, and future research opportunities restricted. Civil and criminal legal punishments can be severe. A rudimentary understanding about human subjects protection and the role of IRBs should be an integral part of ethics training in MS.
History provides useful perspective. The IRB review is part of human subjects protections prescribed by regulations created in response to law. The first regulations protecting human subjects became effective in 1974, and these have been modified and expanded multiple times. The current controlling federal regulations are found at Title 45, Part 46 of the Code of Federal Regulations, and were last revised in 1991; you can find these on the web. The U.S. Federal Policy for the Protection of Human Subjects is known as the "Common Rule" and is widely applicable across federal agencies. There are special protections in place, described in concordant regulations, for research involving fetuses, pregnant women, children, and prisoners. The history of human subjects includes real instances of human subjects abuses that defy both common sense and common decency. The abusers were not only individuals, but also governments.
An IRB overview evaluates proposed research for the adequacy and appropriateness of its human subject protections. Broad general standards against which the proposed research is judged are described in what is called the Belmont Report of 1978 (2), which "sets forth the basic ethical principles underlying the acceptable conduct of research involving human subjects. Those principles, respect for persons, beneficence, and justice, are now accepted as the three quintessential requirements for the ethical conduct of research involving human subjects: 1) Respect for persons involves a recognition of the personal dignity and autonomy of individuals, and special protection of those persons with diminished autonomy; 2) Beneficence entails an obligation to protect persons from harm by maximizing anticipated benefits and minimizing possible risks of harm; and 3) Justice requires that the benefits and burdens of research be distributed fairly."
A hallmark of human subject protection is informed consent. An individual, having been fully apprised of the risks and benefits of the proposed research, agrees to participate. In research that ultimately involves an MS analysis, there is usually no explicit physical risk from the analysis to human subjects. However, garnering the informed consent of involved human subjects means that the goals and procedures of the mass spectrometric analysis, as part of the overall research, should be explained in terms understandable to the general public. Several explanations with increasing levels of detail and depth might be needed. Part of the risk–benefit analysis is to be able to explain the potential benefits in language as clear as the potential risks. "Benefits" might include personal benefits for the individual and also broader societal benefits that are usually thought of as the consequences of research. As MS research and analysis expands into the area of medical diagnosis or the search for disease markers, a definitive "personal benefit" linked with the research or analysis is established. In this instance, the MS data might have a direct personal consequence. Therefore, we must always consider the ethical dimension of MS data.
Again, we start with responsible conduct of research guidelines for data. In general, for any analytical data, these guidelines might describe, for example, how laboratory notebooks are to be kept, and how electronic record keeping should be structured. In protocol-driven analysis, these guidelines can be specific and stringent. In research, with its trial and error, and with a number of false starts early on in the process, the expectations of the relevant research community might be less precise. Certainly, a result worth publishing or presenting is worth repeating under carefully controlled and documented conditions. A rational documents management system, sample inventory system, and instrument file naming system should be in place. Practical measures should be in place to duplicate and archive important records, both on paper and electronically.
For samples that might be linked to particular individuals, large ethical issues have to be considered. Special attention to inventory and naming systems is required. Experimental designers might be familiar with the general concepts of blind and double-blind protocols. However, anonymization of data to ensure a neutral and objective data analysis of the data set is only part of a larger ethical issue — the control and confidentiality of data with predictable consequences for individuals.
Clearly, for proper protection of human subjects, a relevant issue to be considered is the connection between health-relevant data and an individual. Health-related individual information, its control and uses, is the subject of new and evolving laws and regulations. Let's begin outside of the MS laboratory and provide examples of control and uses. A drugstore might stock an array of medically related diagnostic tools and diagnostic kits. For example, a consumer can purchase devices to measure blood pressure or blood sugar. The instructions for use must be clear and unambiguous, and the device must include information on the interpretation of the results obtained. A blood pressure monitor produces numbers as results. The result in this case, however, is not the answer, as we discuss below. An over-the-counter pregnancy test kit is available in the United States. The first pregnancy test kit appeared in 1977, after its maker met the requirements of the 1976 Medical Devices Act as determined by the Food and Drug Administration. The biochemistry behind the text is fascinating (3), but the final result is also the final answer, provided directly as a simple, unambiguous Yes or No. The public has increasingly been afforded access to tools and tests that provide personal information, but the differentiation between results and answers is not always clear.
Consider public access to mass spectrometric information. A consumer with an urge to know can contract with an analytical testing service for a gas chromatography (GC)–MS analysis of the sample of their choice. Testing for hire, by independent experts, is of long antecedent in the legal field. But analytical services using MS are also available to any individuals willing to pay the fee. The service might provide results to the consumer — a complex data set (consider how much data actually constitutes a GC–MS analysis), and some interpretive follow-up. Almost invariably, a conversation ensues in which the consumer wants to know the answer. The point sounds superfluous and obvious, but it is neither. What the consumer purchases from the analytical testing service is a GC–MS analysis. The consumer gets results. What the consumer usually wants, from the service or elsewhere, is an answer.
The connection between the data (the results) and the answer constitutes the essential value of any analysis. We can forge the connection if the question was correctly framed, if the analysis was correctly designed, and if our interpretive experience is sufficiently broad. Return to the example of the results of a blood pressure measurement, and its connection to an answer. An individual result of blood pressure measurement becomes part of a series of measurements that derive value from their placement as consistently above or below average values, as interpreted and established by professionals who evaluate many such measurements from many individuals. The results become an answer only in that context. Contrast this need for connection with the value of the pregnancy test directly providing a simple Yes or No answer. The connection is directly forged because research established a specific and unambiguous marker for pregnancy, and the test is designed to establish the presence of that marker.
A GC–MS analysis of a sample (blood or urine) can be used as a screening tool for early indications of an altered biochemistry. The pattern of the results, especially as established over a period of time, is interpreted in the perspective of other results to provide an answer. The GC–MS analysis is analogous to the blood pressure measurement described above. In the case of an established disease marker, with the appropriate validation, the MS result instead might be a Yes or No answer, as in the pregnancy test. A tension develops between the need for careful validation and the seemingly insatiable demand for nearly instant unambiguous answers. The ethics component is added because in either case, the data are linked to an answer and the answer is linked to an individual. When does research evolve into an analysis that should be available to the public on demand? Should the availability of analysis be restricted to those with professional expertise, such as the medical profession, or should it be available to individuals? These are the broader ethical issues of information; or to coin a term, this is informethics.
Does informethics matter now? On August 26, 2008, the New York Times described a new blood test to detect ovarian cancer at an early stage when the prospects for treatment are most promising (4). The test, which measures the levels of six "diagnostic" proteins in blood, is available to the public through their physicians. But the regulatory authority over this particular test is apparently unclear, and the validity of the answers indicated by the results is under debate, while the substantial personal impact is already documented in the article. On August 29, 2008, the Los Angeles Times described a DNA database that was available over the web to facilitate research (5). This database contained the genetic information of approximately 60,000 patients. The IRB review required, and the informed consent indicated, that the patients' profiles were anonymous. The article describes the discovery that the anonymity of the patients was not as "protected" as originally thought, even with the careful controls put in place. It was discovered that the individual patients could be linked to their specific medical conditions and therefore identified. The database was taken offline. Informethics must be considered now.
MS data have almost always been used previously to tell us about things — elements and their isotopes, organic molecules and their structures, mixtures and their components. First, we had data, and then data collected into databases, and then we began to take full advantage of the higher dimensions of data through informatics. MS is now being used to tell us about ourselves, and about single identifiable individuals — their health, their diseases, their potential diseases, what they have eaten, what they smoked, and what they have touched. Information generated by MS now must be evaluated in an ethical environment that considers factors of confidentiality, control, certification, and even culpability. Each factor is linked under the umbrella of ethical conduct of research, and the ethical conduct of scientists.
We should exert some self-control in the creation of titles and the composition of abstracts for our papers and our presentations, knowing that web searches are both easy and pervasive. Responsible ethics should steer us away from self-serving publicity, and from promise of the silver bullet or the miracle cure. We must also be aware that the public views our words, and our science, with a nonscientific eye; that the publicist's goal is publicity and not scientific validity; and that the timely iterative progress of science, and of validation, testing, and certification, should be central to our own scientific ethics.
Kenneth L. Busch
predicts that small time-of-flight mass spectrometers will soon occupy the bench space in the instrument room at the medical clinic. Quick 5-min test kits will process samples from individual patients and provide a sample surface optimized for laser desorption, or desorption electrospray ionization. Microorganisms leading to infections might be so identified, and the data might provide preliminary positive or negative indications for disease markers. Interpretation of such personally identifiable data will then be completed with heuristic systems. The promise of such technology is confounded by an incomplete understanding and expectation of who controls, and who has access to, such data. KLB can be reached at wyvernassoc@yahoo.com.
References
(1) S.A. Carr, M. Gillette, T. Addona, H. Keshishian, M. Burgess, V. Sanz-Vash, K.R. Clauser, and R. Kumm, "Progress toward a Biomarker Discovery-to-Development Pipeline in Clinical Proteomics," Presented at the 56th Annual Conference on Mass Spectrometry, Denver Colorado, June 1–5, 2008.
(2) http://www.hhs.gov/ohrp/irb/irb_introduction.htm
(3) http://history.nih.gov/exhibits/thinblueline/timeline.html
(4) A. Pollack, "Cancer Test for Women Raises Hope, and Concern," New York Times, August 26, 2008.
(5) J. Felch, "DNA Databases Blocked from the Public," Los Angeles Times, August 29, 2008.
Newsletter
Get essential updates on the latest spectroscopy technologies, regulatory standards, and best practices—subscribe today to Spectroscopy.
New Study Expands Nickel Autoionization Spectra to Advance Laser Isotope Separation Technologies
July 17th 2025Researchers at China’s National Key Laboratory have identified 170 nickel autoionization states using resonance ionization mass spectrometry, significantly advancing the spectral database critical for laser isotope separation and atomic spectroscopy.
A Life Measured in Peaks: Honoring Alan George Marshall (1944–2025)
June 18th 2025A pioneer of FT-ICR Mass Spectrometry, Alan G. Marshall (1944–2025), is best known for co-inventing Fourier transform ion cyclotron resonance mass spectrometry (FT-ICR MS), a transformative technique that enabled ultrahigh-resolution analysis of complex mixtures. Over a career spanning more than five decades at institutions like the University of British Columbia, The Ohio State University, and Florida State University, he published over 650 peer-reviewed papers and mentored more than 150 scientists. Marshall’s work profoundly impacted fields ranging from astrobiology to petroleomics and earned him numerous prestigious awards and fellowships. Revered for his intellect, mentorship, and dedication to science, he leaves behind a legacy that continues to shape modern mass spectrometry.
The Role of LIBS in ChemCam and SuperCam: An Interview with Kelsey Williams, Part III
May 2nd 2025In this extended Q&A interview, we sit down with Kelsey Williams, a postdoctoral researcher at Los Alamos National Laboratory (LANL), who is working on planetary instrumentation using spectroscopic techniques such as laser-induced breakdown spectroscopy (LIBS) and laser ablation molecular isotopic spectrometry (LAMIS). In Part III, Williams goes into detail about ChemCam and SuperCam and how LIBS is used in both these instruments.