Using Infrared Spectroscopy for Real-Time Diagnostics During Brain Surgery
What if the decisions neurosurgeons make during surgery - such as about how much tissue to remove - could be guided by immediate results from spectroscopic methods? A number of spectroscopy researchers are seeking to advance methods to make that both possible and practical.
What if the decisions neurosurgeons make during surgery — such as about how much tissue to remove — could be guided by immediate results from spectroscopic methods? A number of spectroscopy researchers are seeking to advance methods to make that both possible and practical. One such researcher is Allison Stelling, who recently completed her PhD under Professor Peter Tonge at Stony Brook University in New York. Stelling is currently at the Center for Materials Genomics at Duke University, in Durham, North Carolina, working under Professor Stefano Curtarolo. Previously, during a post as a scientific research associate in the Clinical Sensing and Monitoring department in the Faculty of Medicine at Dresden University of Technology, in Dresden, Germany, Stelling and colleagues studied the use of infrared (IR) spectroscopy for use in intraoperative diagnostics during brain surgery. Spectroscopy recently spoke to Stelling about that work, which was published in the journal PLoS ONE (1).
When using IR spectroscopy to examine freshly resected brain tissue in an operating room, what are you trying to achieve?
The end goal is to be able to detect the hard-to-see tumor borders during operations, because incomplete removal is linked to recurrence in many brain tumors. In soft tissues like the brain, these borders shift during the operation from preoperative magnetic resonance imaging (MRI) images. IR can give contrast in these low-contrast situations, and thus aid in reducing the number of surgeries a patient must endure. This initial study was focused more on determining where reliable spectral differences are between normal and tumor in fully hydrated tissue. Further studies will be needed to see how the identified signals "titrate" between normal and tumor tissue.
When analyzing brain tumors with IR spectroscopy, what biomarkers are you measuring? How precisely can these markers be differentiated in healthy and cancerous tissue, and to what extent do individual variances occur? Have the biomarkers been validated?
Chemicals produced by the tumor itself and then sensed by IR serve as the biomarkers. In the attenuated total reflectance Fourier transform infrared (ATR-FTIR) spectra from tumor tissues, this results in fairly dramatic shifts in frequency and changes in absorbance. While full interpretation on a chemical level must await purification and structural characterization studies, it is apparent that there do seem to be reasonably large changes in the ATR-FTIR between the control brain tissues and the tumor ones.
In our recent study , we found a particular region that contains signals from extracellular molecules like collagen, whose triple helix structures give it a very distinctive IR signal. Collagens are overexpressed in many tumors, resulting in large changes in the IR. These changes were plotted in the recent paper we published in PLoS ONE (1). Dr. Deirdre Toher, a statistician at the University of the West of England in Bristol, helped me with some of the basic spectral preprocessing in large batches for the study.
A major lesson I gained from this trial — and when doing my literature survey for the recent publication — addresses your question about how to identify so-called "spectral biomarkers" or "fingerprints" for disease. Doing controls with healthy tissues and comparing and contrasting them with diseases can allow us to first determine where reliable differences occur. Comparison with tissues known to overexpress certain chemicals can help assign bands and determine roughly their percent contribution to the overall tissue spectrum.
Inter-individual variance for this measurement was something I was quite concerned about, which is why Dr. Ordtrud Uckermann, a neuroscientist at the Department of Neurosurgery in the Dresden University Hospital, and I designed a small control study to obtain the IR signals from normal, healthy mouse brains. The variation among the five individual animals was much lower than I expected it to be (particularly for waterlogged materials), and forthcoming manuscripts on this trial will illuminate this point.
What will be most interesting to see is how the IR spectra change between patients with the same diagnosis using traditional histochemistry. IR shall likely be much more sensitive to intrinsic, biochemical-level inter-individual differences in the phenotype of the tumor than any morphology-based method. This information will help biomedical scientists in the future design personalized treatments with physicians based on a patient's unique biochemistry.
This is the preclinical trial, so validation is the next step. These initial results are reasonably promising, however, and illustrate that the core idea is sound.
You used a portable IR instrument with an ATR device with a particular beam path. What are the advantages of that beam path?
The major technical advantages of the ATR beam path lie in the ease of measurement it allows (no sample preparation is needed, just firm contact with the crystal) and the low penetration depth of the beam, which reduces the signal from water in freshly harvested tissues and living cell cultures.
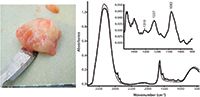
Figure 1: Left: A typical piece of resected human brain tumor tissue. Right: The ATR-FTIR spectrum of freshly resected brain tissue (solid) overlaid with the spectrum from a pH 7.5 isotonic buffer (dashed).
Another nice feature of the ATR beam path is that it measures an averaged signal — slight alterations due to healthy fluctuations in cellular metabolism do not appear to affect tissue spectra. Dramatic changes in biochemistry such as those that occur during pathogenesis need to occur for the signal to alter. Thus, it is less prone to measure the "noise" that more sensitive instrumentation may pick up on in living systems.
Most IR studies of tissues are performed on dried specimens. When looking at fresh, hydrated tissues, how do you avoid having the strong IR signal of water overwhelm the signals from biochemicals in the tissues?
As mentioned above, the ATR beam path is quite short —usually only a few micrometers, depending on the material. This reduces the water contribution to the signal, and compression with the anvil helps enhance the signals from the biochemicals. This is a fairly well known physical effect that was discovered in the 1960s (2). Advances in the optics over the years have produced much more robust beam paths and detectors that yield quite reproducible spectra with good signal-to-noise ratios.
What challenges have you had to overcome to apply IR spectroscopy to intraoperative diagnostics? What challenges remain?
Overcoming the challenge of the IR water signal was the first thing we sought to address. When I first went into Dresden University Hospital's operating room (OR) in 2009, my boss at the time, Professor Emeritus Reiner Salzer, of TU Dresden's Department of Bioanalytical Chemistry, asked me point blank if I were controlling for water in these "IR in the OR" experiments. The ORs are frequently not temperature-regulated in the same way instrumentation laboratories are, and humidity alone can be an issue, along with many other factors. To address this excellent question, Dr. Uckermann and I designed a small control study with normal mouse brain tissue. That study was carried out by her and one of the students, Holger Cramm. As a consummate neuroscientist, Dr. Uckermann can remove a mouse brain from a living animal in under 3 min. That study replicated the conditions that the patient tissue would be under and provided normal brain tissue data to serve as a sort of control. I intended the PLoS ONE paper to be a solid methodology paper. Forthcoming manuscripts will illustrate that the replicability of this ATR-FTIR measurement is somewhat surprising for such heterogeneous, hydrated materials.
One of the major challenges remaining is explaining to the medical doctors how to interpret the data obtained from IR measurements. The team in the Department of Neurosurgery at the Dresden University Hospital is unique in the world as it has a spectroscopist, Dr. Gerald Steiner, and a neurosurgeon, Dr. Matthias Kirsch, both working on bringing this technology out of the lab and into the operating room. However, communicating this field as a whole to a broad medical audience will be challenging. Physicians and life scientists take very different courses in their training than physical scientists do, and this can make cross-disciplinary communication difficult.
What results have you obtained so far?
Thus far, we have determined a solid method for reducing the water signal, which seems to yield reliable measurements between identically prepared and fully hydrated biological samples. After comparing all the data sets — cells, animals, and human tumors — I located a particular region that appears to change reliably when going from normal to tumor tissue. Further trials will have to be orchestrated to confirm and enhance this initial data set.
How difficult is it for medical staff to use the results from spectroscopic analysis quickly during surgery?
Currently, the surgeon would have to have a spectroscopist familiar with tissue IR interpretation in the operating room — and clearly this is not a viable option for the future. I did the analysis the old-fashioned way for this preliminary paper: I went through all the spectra that my undergraduate thesis student Jelena Tavkin (who is currently in a biophysics master's program at the Max Planck Institute of Molecular Cell Biology and Genetics in Dresden) and I collected, and then found regions in the patient IRs that had clear, bulk alterations in frequency or absorbance from the control mouse spectra. Easy-to-use software will have to be designed explicitly for medical users — physicians do not have time during operations to think about complex analysis.
References
(1) A.L. Stelling et al., PLoS ONE 8(3), e58332 (2013). doi:10.1371/journal.pone.0058332
(2) N.J. Harrick, Phys. Rev. Lett. 4, 224–226 (1960).

AI Shakes Up Spectroscopy as New Tools Reveal the Secret Life of Molecules
April 14th 2025A leading-edge review led by researchers at Oak Ridge National Laboratory and MIT explores how artificial intelligence is revolutionizing the study of molecular vibrations and phonon dynamics. From infrared and Raman spectroscopy to neutron and X-ray scattering, AI is transforming how scientists interpret vibrational spectra and predict material behaviors.
Real-Time Battery Health Tracking Using Fiber-Optic Sensors
April 9th 2025A new study by researchers from Palo Alto Research Center (PARC, a Xerox Company) and LG Chem Power presents a novel method for real-time battery monitoring using embedded fiber-optic sensors. This approach enhances state-of-charge (SOC) and state-of-health (SOH) estimations, potentially improving the efficiency and lifespan of lithium-ion batteries in electric vehicles (xEVs).
New Study Provides Insights into Chiral Smectic Phases
March 31st 2025Researchers from the Institute of Nuclear Physics Polish Academy of Sciences have unveiled new insights into the molecular arrangement of the 7HH6 compound’s smectic phases using X-ray diffraction (XRD) and infrared (IR) spectroscopy.